
50 to 60% of depressed individuals also report suffering from chronic pain, a finding that is the main motivation for many studies that attempt to explain the link between these two sources of sadness, particularly by trying to understand To what extent one can enhance or even excite the other. In a study to understand the effects of chronic pain on mood and depression, researchers have shown for the first time in humans that chronic pain is associated with decreased levels of GABA (an inhibitory neurotransmitter). In other words, chronic pain has a disruptive effect on the chemical functioning of a part of the brain involved in mood.
New study shows how chronic pain affects the way our prefrontal lobes process emotions at a fundamental level, and shows that the tendency to become more anxious or depressed is the result of a disruption in the way cells communicate. , which contains inhibitors of the neurotransmitter GABA.
« Chronic pain is more than a terrible feeling Sylvia Gustin, a neuroscientist and psychologist at the University of New South Wales and a neurological research institute in Australia, tells Neura. ” It can affect our feelings, beliefs, and the way we are Adds the lead author of the new study.
Chronic pain: profound effects on brain function
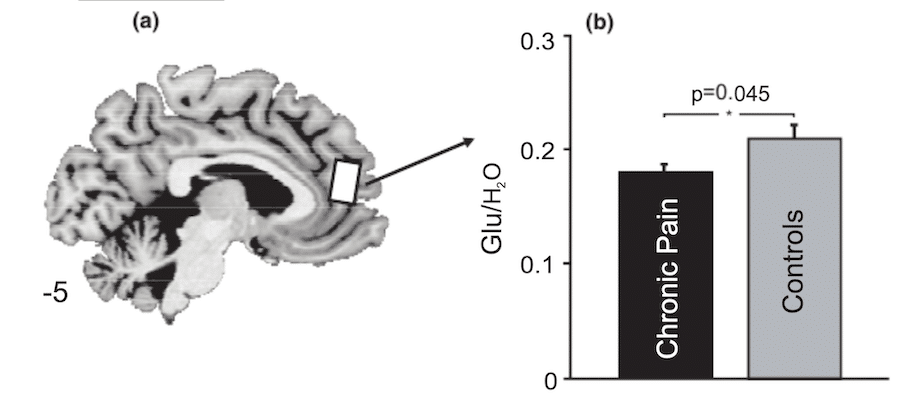
Gustin and his colleagues used advanced imaging techniques to look at the concentrations of a specific neurotransmitter in volunteers with and without a history of chronic pain. This neurotransmitter, gamma-aminobutyric acid (GABA), is one of the main players in brain signaling, which controls neuronal activity throughout the nervous system.
Specifically in the brain’s prefrontal cortex, the moderating activity of GABA acts as a form of “traffic control”, limiting communication with other regions such as the amygdala. In balance with glutamate, an excitatory neurotransmitter, this signaling system allows our emotions to prompt us at just the right time without causing us excessive stress.
Traumatic situations can be seen as the perfect time to release our emotions, whether to encourage help or to help us free ourselves. Studies in animal models have shown significant changes in the amount of glutamate present in the central region of the prefrontal cortex when subjects are in pain. Similarly, the researchers found that humans with chronic pain had decreased amounts of glutamate, along with a decline in their emotional regulation.
However, if changes in the amount of GABA were observed in rats, this link had not yet been established in humans. Knowing whether a neurotransmitter directly responsible for “turning off the flood” of our deepest feelings of anxiety is missing when we are in pain can help us better understand not only our brains, but people’s lives. may also pave the way for new treatments aimed at helping With depression related to chronic pain.
GABA levels: a direct effect in the feeling of pain
In a sample of 48 participants with and without chronic pain, brain scans revealed significant contrasts in GABA levels. While the number of volunteers isn’t huge, it is enough to support the idea that reducing long-term pain inhibitory measures alters the way our brains process emotions.
« We have shown for the first time in humans that sustained pain is associated with a decrease in GABA, an inhibitory neurotransmitter in the middle prefrontal cortex. In other words, there is an actual pathological change that occurs. Gustin says. The results of the study were published inEuropean Journal of Pain. Without GABA, the “calculations” made in the anterior part of our brain are enhanced, which not only processes our emotional responses, but our rational thoughts and actions.
Every year, one in ten people in the world experiences some degree of chronic pain, a problem that affects more people than heart disease, diabetes and cancer combined. In some areas this figure reaches even one in four people.
Given the frequency of this experience, we should learn more about ways to deal with its worst effects. Mood disorders and chronic pain have long been known to go hand in hand, with up to half of people with painful episodes lasting more than a few months also suffering from depression or anxiety.
The consequences can be dire: disturbed sleep, stress and feelings of guilt. Targeting specific changes in neurochemistry to such a small area of the brain is a challenge, especially when neurotransmitters such as glutamate and GABA have such widespread effects in the nervous system.
But knowing that the physical changes that link chronic pain to emotional management can help affected people gain some perspective and some control over their bodies. ” The brain cannot reduce these feelings on its own, but it is plastic – and we can learn to change it. Gustin says. These results are therefore a source of hope for the development of new treatments.
